Moving on From Traditional Insurance Processing with AI
Insurance in the United States is a trillion dollar industry, playing a role in nearly every other industry on the planet. It is an integral part of our society and economy, which is why there is a great need...
Insurance in the United States is a trillion dollar industry, playing a role in nearly every other industry on the planet. It is an integral part of our society and economy, which is why there is a great need for a modernization of the framework and processes. Currently, there is no efficient and effective method for capturing, verifying, and processing insurance that is consistent with the technological development of the rest of our society. The in-place traditional methods hold several problems, robbing companies and policy holders of their time, money, and accuracy.
Denied claims are very common in this industry, and they are far more costly than many are aware of. For example, health insurance denied claims equal over $262 billion annually. In addition, 27% of all denied claims in this sector, equating to over $70 billion, result from errors at patient registration during insurance processing. To put this into perspective, this $71 billion is 1/60 of all healthcare spending in the United States, and is more than the annual Medicaid expenditures in nearly all of the US states. These numbers more than illustrate the need for improvements in order to save money and valuable assets.
There are several contributors to these shortcomings of the industry, all pointing back to the general limitations of the traditional methods we currently rely on. Most existing OCR solutions to insurance processing cannot identify insurance information that is not printed on a physical insurance card. This excludes the ability to process any digital cards, which have become the norm in this digital age. More and more patients are downloading their cards online for ease of use, which eliminates the ability for scanning and processing with technology. In addition, some providers like Medicaid, Blue Cross Blue Shield, and Medicare do not even print payer IDs on cards, which means that human intervention is then required. Not only is this inconvenient for busy providers, but it also requires highly trained individuals to be put to work. This expertise, once obtained, is slower than the capabilities of technology, and leaves more room for potential error.
Traditional insurance capture is prone to error due to the large amount of human intervention that is required to complete the process. For example, 19.3% is the current average error rate among all health insurance in the United States. When put into the perspective of the sheer volume of insurance plan holders in the country, this percentage can be seen as detrimental. On top of these limitations, there is also the problem of locality that plagues many insurance companies. Many large providers have state, local, and ZIP claim processes that require one to select a specific locality. This process requires a knowledge of several pieces of information that may be difficult to obtain. When one fails to properly identify and provide this information, a denied claim is likely, costing the holder and company time and money.
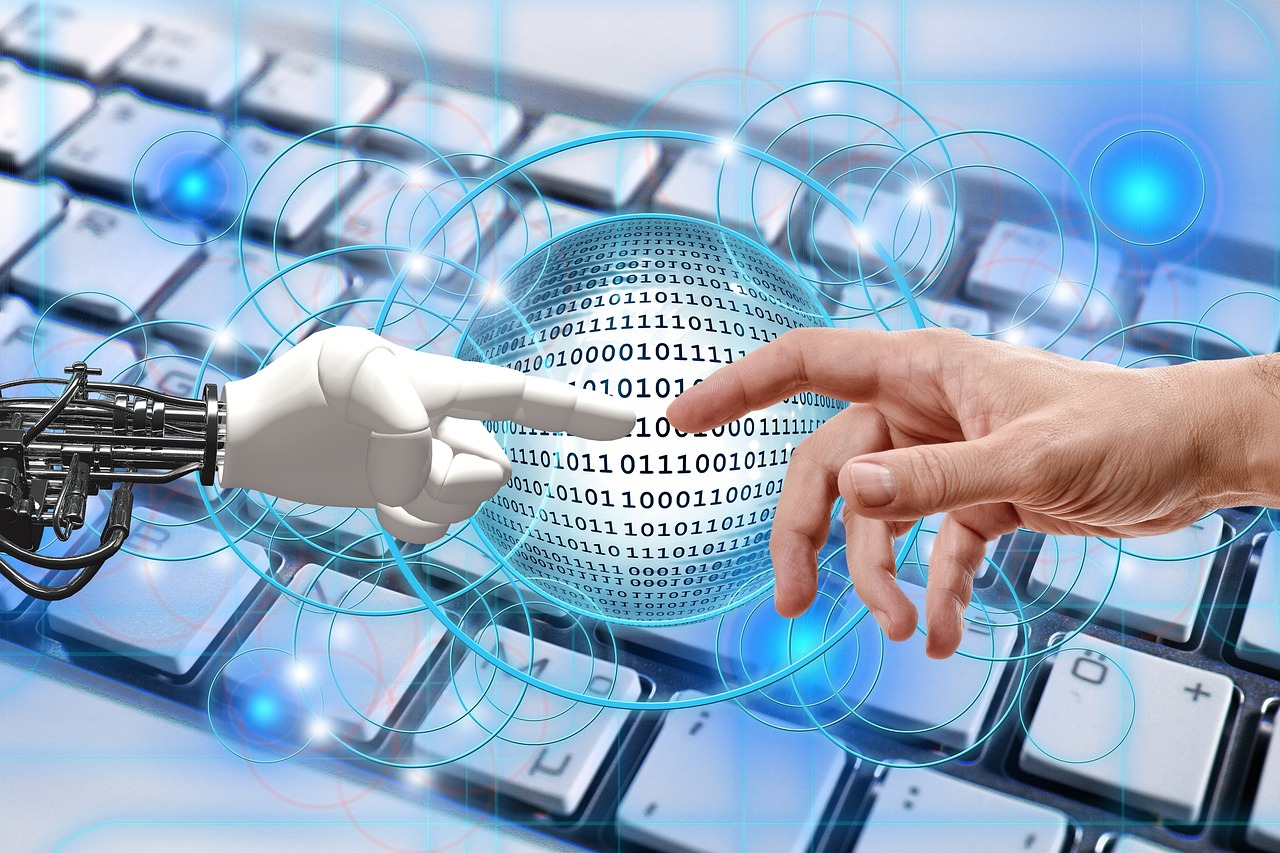
Without technology, there is no way to completely eliminate pitfalls like misidentification, incorrect data entry, or any inaccuracies throughout the process. It is for these reasons that experts are working on a new and improved way to carry out these processes. An AI-powered solution is in the works, processing insurance like a human without the chance for error. The new technology is an insurance card reading artificial intelligence model that is trained on thousands of insurance payers and hundreds of thousands of plan types. This works in tandem with advanced algorithms that validate information and important details in less than seconds. This program would be able to identify plan details as well as pharmacy insurance details in real time, making this the most advanced model of its kind.
The benefits speak for themselves, as what traditional methods could do in minutes, AI can do in seconds. In addition, every reworked claim due to errors costs providers an average of 25% per claim. However, AI can save up to 80% for providers with this new reliable technology. Artificial intelligence is easily trained to remain up to date with new needs, while medical staff may have limited experience or need time to become knowledgeable. Finally, there is no need to worry about human needs like employee burnout or turnover. Artificial intelligence can help alleviate workload and improve the quality of work amongst human staff.
There is no doubt that the future is bright for the insurance industry. Despite the current lack of modernity, there is hope in early developments of a more optimal alternative. While old methods may be inefficient, slow, inaccurate, and tedious, new technology has the power to move at greater speeds and with less error than ever before. Gone are the days of denied claims and costly mistakes, as the industry welcomes artificial intelligence as the new most important player in insurance processing.

 Tfoso
Tfoso