HIV-positive people who have monkeypox are hospitalized more often, CDC study says
The CDC found that 38% of nearly 2,000 people diagnosed with monkeypox between May and July were living with HIV.
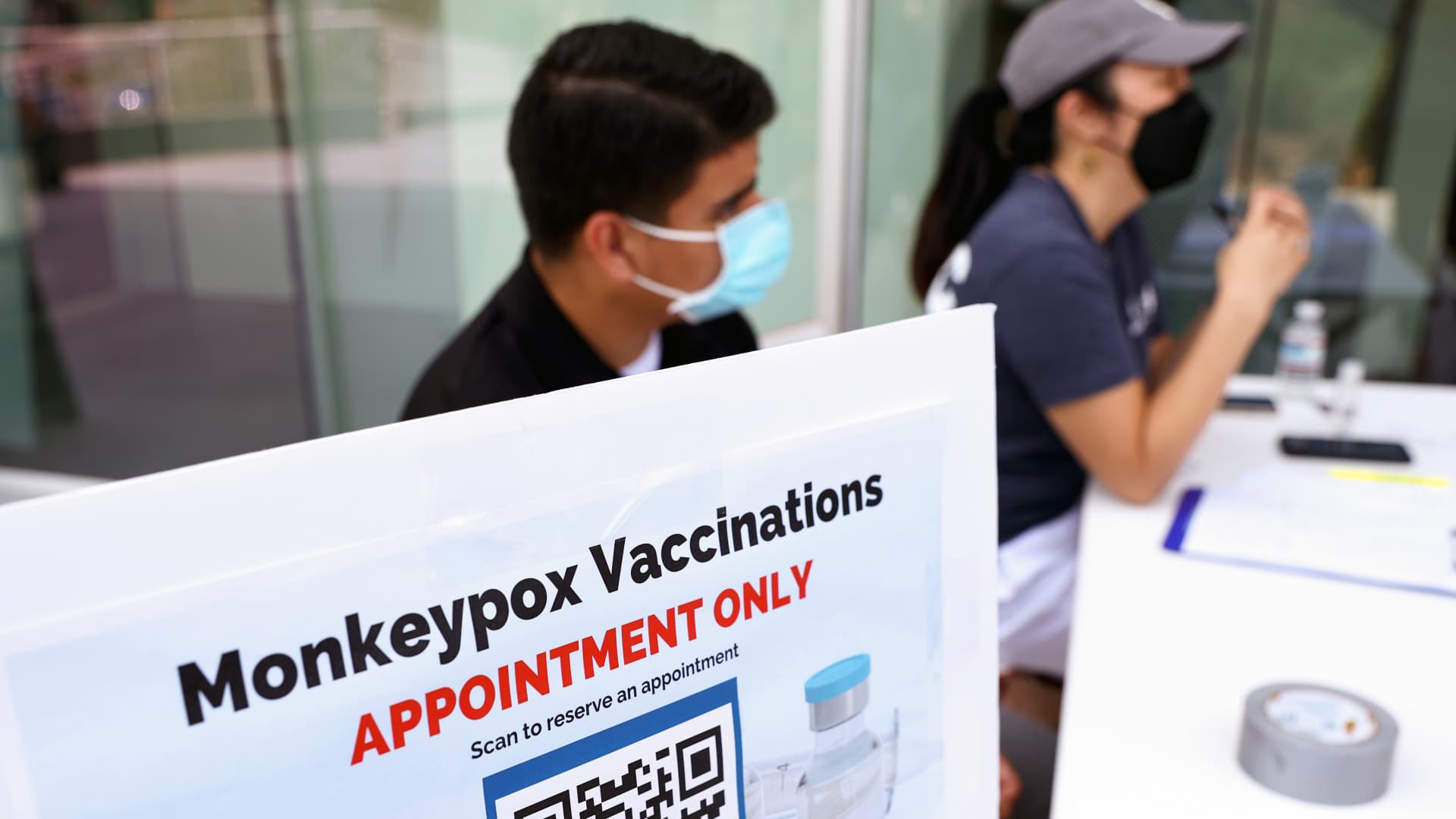
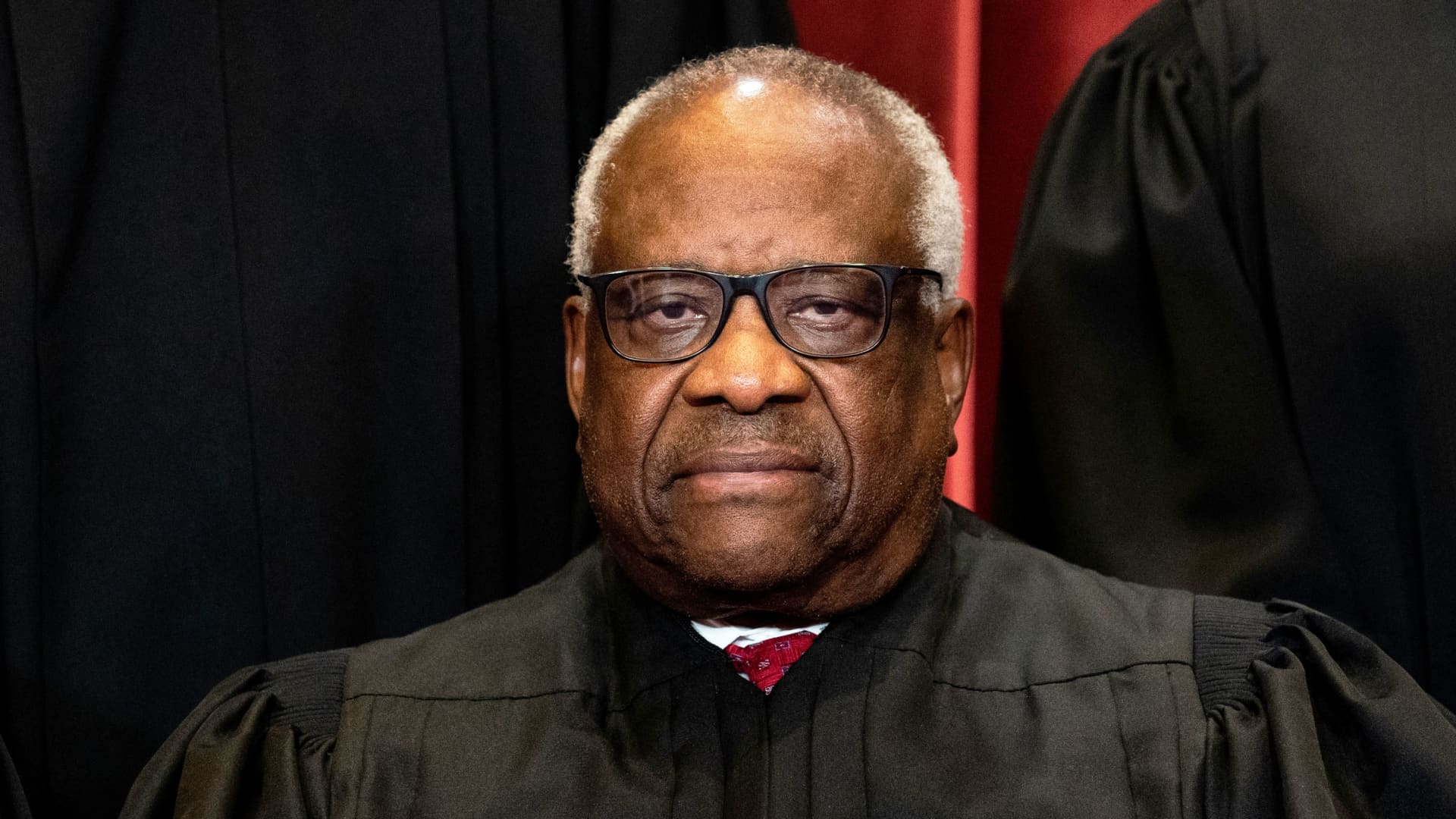
Health workers sit at a check-in table at a pop-up monkeypox vaccination clinic which opened today by the Los Angeles County Department of Public Health at the West Hollywood Library on August 3, 2022 in West Hollywood, California.
Mario Tama | Getty Images
People living with HIV who have monkeypox are hospitalized more than twice as often as other patients diagnosed with the rapidly spreading virus, according to a study from the Centers for Disease Control and Prevention.
In a report published Thursday, the CDC found that 38% of nearly 2,000 people diagnosed with monkeypox between May and July were living with HIV. Among 1,300 monkeypox patients with more detailed clinical data, 8% of HIV-positive individuals were hospitalized compared with 3% of people without HIV infection.
The CDC found that HIV-positive individuals in particular with low T-cell counts, which indicates a weaker immune system, and in whom the virus is not suppressed are hospitalized more frequently with monkeypox.
But data on the reason for hospitalization is incomplete so it's unknown whether HIV-positive people hospitalized with monkeypox are suffering from more severe disease, according to the CDC. People living with HIV in previous monkeypox outbreaks in Nigeria did have poor outcomes.
Monkeypox is primarily spreading during sex among gay and bisexual men, though anyone can catch the virus through close physical contact with someone who is infected or contaminated materials such as towels and bedsheets.
Men who have sex with men have HIV infections more often than the general population, according to the CDC. But the 38% of monkeypox patients who also have HIV is far higher than than the rate observed among the broader population of gay and bisexual men, the study found.
The percentage of monkeypox patients who have HIV has also increased over time, which suggests monkeypox may be spreading more in networks of people who have HIV, according to the agency.
The CDC found a major racial disparity among people who have HIV and monkeypox. Black and Hispanic patients had monkeypox and HIV at a far higher rate – 63%, and 41% – respectively, than white patients at 28%.
Monkeypox is disproportionately impacting Black and Hispanic populations. Nearly 38% of monkeypox patients are Black, 29% are Hispanic and 27% are white, according to CDC data. The overall U.S. population is 12% Black, 19% Hispanic and 61% White, according to data from the 2020 Census.
People with HIV who also have monkeypox are reporting some symptoms more often such as rectal pain and proctitis. Monkeypox causes a rash, which resembles pimples or blisters, that often develops on sensitive areas such as the anus or genitals.
The CDC officials who authored the study said vaccination against monkeypox should be prioritized for people who are HIV-positive and who have other sexually transmitted infections.
People evaluated for monkeypox should also undergo HIV and STI screening, the authors said. Some 41% of monkeypox patients were diagnosed with one or more STIs over the past year, according to the CDC study. Health-care providers should also offer patients medication such as PrEP, which helps lower the risk of getting HIV through sex.
The CDC has estimated that 1.6 million gay and bisexual men who are HIV-positive or who are taking medication to reduce their risk of HIV face the highest threat from monkeypox. More than 460,000 monkeypox vaccine doses have been administered so far. Department of Health and Human Services officials have said the U.S. is approaching the point where there are enough doses available to fully vaccinate the highest-risk population.
The U.S. is battling the largest monkeypox outbreak in the world, with more than 21,000 cases reported across all 50 states, Washington D.C., and Puerto Rico, according to CDC data. White House health officials said Wednesday that the outbreak appears to be slowing as vaccinations ramp up, though the racial disparity in people diagnosed with monkeypox is growing.

 ValVades
ValVades