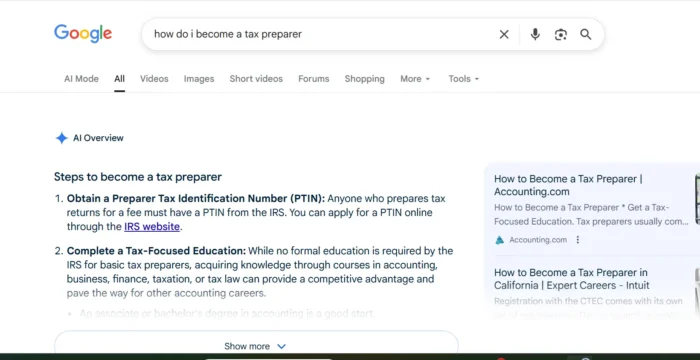
U.S. plans to stop buying Covid shots for the public this fall. Here's what that means
Under the Affordable Care Act, most Americans would still get their Covid shots for free once the vaccine program goes commercial.

A pharmacist delivers a COVID-19 booster dose at a Chicago CVS store in October.
Antonio Perez | Tribune News Service | Getty Images
The U.S. will stop buying Covid shots at reduced price for the entire country and shift vaccine distribution to the private market as soon as early fall, shifting the cost to U.S. insurers and uninsured Americans who stand to lose access to the free vaccines.
Dr. Ashish Jha, the White House Covid response coordinator, said in an an interview with UCSF Department of Medicine on Thursday that the shift to a private market will happen over the summer or early fall, though no exact date has been set.
A senior official with the Health and Human Services Department told CNBC the fall would be a natural time to transition to a private market, particularly if the Food and Drug Administration selects a new Covid strain for the vaccines and asks the manufacturers to produce updated shots ahead of the respiratory virus season.
For the past two years, the U.S. has bought the vaccines directly from Pfizer and Moderna at an average price of about $21 per dose, according to the Kaiser Family Foundation.
The federal government has required pharmacies, doctor's offices and hospitals to provide these shots for free to everyone regardless of their insurance status.
If you have health insurance
When the federal Covid vaccination program ends, the shots will remain free for people who have health insurance due to requirements under the Affordable Care Act.
But uninsured adults may have to pay for their immunizations when Pfizer and Moderna start selling the shots on the private market and the current federal stockpile runs out. There is a federal program to provide free vaccines to children whose families or caretakers can't afford the shots.
Jha said on Tuesday the planned switch is not tied to the end of the Covid public health emergency in May.
"The end of the PHE does NOT mean people will suddenly not be able to get the vaccines and treatments they need," Jha wrote in a Twitter thread on Tuesday.

When the federal government no longer buys vaccines at a discount for the entire nation, individual health-care providers will purchase the shots from the vaccine makers at a higher price.
Moderna CEO Stephane Bancel told CNBC last month that the company is preparing to sell the vaccines on the private market as early as this fall. Pfizer CEO Albert Bourla told investors during the company's earnings call this week that he is preparing for the vaccines to go commercial in the second half of the year.
Pfizer and Moderna have said they are considering hiking the price of the vaccines to somewhere around $110 to $130 per dose once the U.S. government pulls out of the vaccine program.
If you're uninsured
"If you're uninsured, then you might be faced with the full cost," said Cynthia Cox, an expert on the Affordable Care Act at the Kaiser Family Foundation.
But the U.S. still has a substantial stockpile of free vaccines left. The Biden administration ordered 171 million omicron boosters last year. About 51 million boosters have been administered so far, according to the Centers for Disease Control and Prevention.
The uninsured will continue to have access to these 120 million doses for free, but it's unclear how long the supply will last.
"With the supply we have of vaccines and antivirals, we don't think we're going to be in a state of precipitous transition to drop this on market partners," the HHS official said.
Although the vaccine makers are preparing to sell shots on the private market later this year, it's possible that the federal stockpile of free shots could last longer than that because booster uptake has been low, Cox said.
"Everyone in the U.S. regardless of their citizenship status or their insurance status is able to get a free vaccine as long as this federal stockpile lasts," Cox said.
Sen. Bernie Sanders, I-Vt., slammed the vaccine price hike in a letter to Moderna's CEO last month. Sanders, who will chair the Senate health committee, said the price hike would cost taxpayers billions via its impact on Medicaid and Medicare's budgets.
"Perhaps most significantly, the quadrupling of prices will make the vaccine unavailable for millions of uninsured and underinsured Americans who will not be able to afford it," Sanders said. "How many of these Americans will die from Covid-19 as a result of limited access to these lifesaving vaccines?"
Jha said this week that the Biden administration is committed to helping the uninsured access Covid shots and treatments.
"We are creating a whole separate set of efforts for the uninsured because the uninsured, of course, will not be able to get vaccines for free and treatments for free under the regular insurance system by definition," Jha said Thursday. "We are working on a plan on that."
The HHS official said one tool the federal government plans to use is a program called Section 317 that provides funding to procure and administer shots to uninsured adults at no cost.
ACA requirements
But for the overwhelming majority of people with private insurance, the Affordable Care Act will cover the cost of the vaccines. Under the ACA, private health insurance is required to cover all immunizations recommended by the CDC at no cost to the consumer.
Medicare would cover the shots for seniors, who are the most vulnerable to the virus, and lower-income people could get the vaccine through Medicaid.
There may be a small number of legacy private health insurance plans from before the ACA that are not required to cover Covid vaccines, Cox said. The HHS official said most of those plans will likely pay for the shots.
In addition, some short-term insurance policies might not pay for the vaccines, Cox said. These plans were created during the Trump administration and aren't required to comply with the ACA.
The ACA also allows private insurance to limit vaccine coverage to in-network providers, Cox said. People who have grown accustomed to getting vaccinated at any pharmacy during the pandemic might have to go to a specific drugstore in the future to get a free shot, she said.
Consumers could also see their health insurance premiums increase if Pfizer and Moderna hike the price of the shots, Cox said.
Paxlovid may not be free
Some patients, depending on their insurance policy, will also probably have to pay for Pfizer's antiviral pill Paxlovid in the future. Unlike preventive services such as vaccines, the ACA does not require insurance to cover treatments.
Bourla told market analysts this week that Pfizer expects to start selling Paxlovid through the private market at commercial prices in the second half of 2023.
Pfizer has not announced how much the antiviral will cost once it goes commercial. The federal government is paying about $530 for a five-day treatment course. It's unclear how much patients will have to pay out of pocket and how much of the price insurance will cover.
Dawn O'Connell, who heads the federal office responsible for the U.S. stockpile, said last August that the Health and Human Services Department expected to run out of Paxlovid by mid-2023.
Jha said on Tuesday that there are still millions of doses of Paxlovid and omicron boosters in the U.S. stockpile. "They will continue to be available for free to all Americans who need them," Jha said of the remaining federal supply.

 MikeTyes
MikeTyes