7 Dentist-Approved Habits to Prioritize Your Oral Hygiene—and Protect Your Gut
Insights into the surprising connection. The post 7 Dentist-Approved Habits to Prioritize Your Oral Hygiene—and Protect Your Gut appeared first on Camille Styles.

At its core, the human body is a compilation of systems. And while each carries out a unique role, nothing exists in a vacuum. Each system depends on one another to function optimally. That’s why, as digestive health gains more mainstream interest, the relationship between gut health and oral hygiene is garnering further attention in the medical community and beyond. Said differently: to feel your best, the gut health-oral hygiene connection should be top of mind.
Otherwise known as the mouth-gut axis, this process defines the movement of microbes traveling from the oral cavity to the gut. As Dr. Kami Hoss, dentist, orthodontist, and dentofacial orthopedist notes, this process takes place “with every swallow, potentially influencing gut health.”
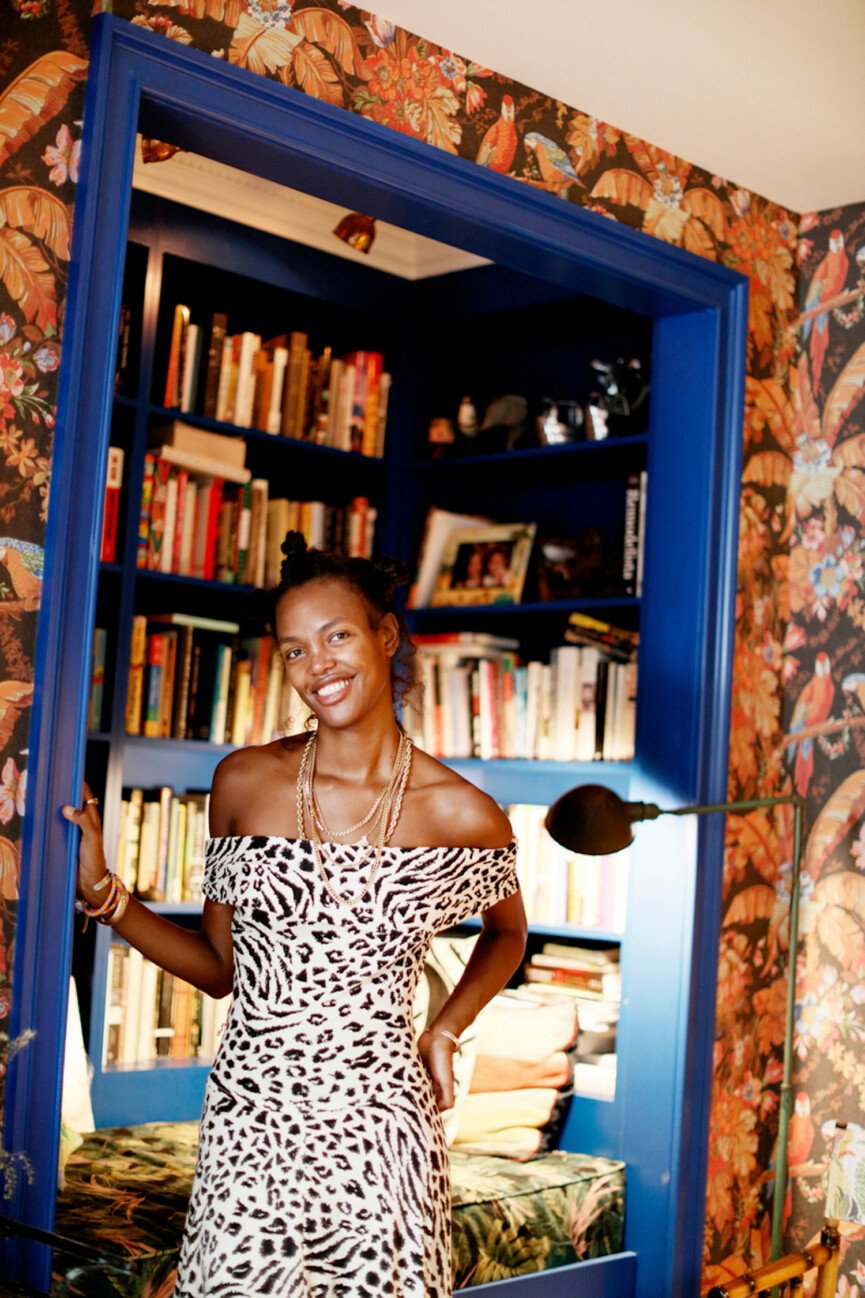
Featured image from our interview with Mary Ralph Bradley.

Understanding the Gut Health-Oral Hygiene Connection
While information is becoming more widespread and accessible on the gut, public knowledge of the oral microbiome is lacking. To further understand this profound and influential exchange, I spoke with Dr. Hoss about all things gut health and oral hygiene.
Ahead, learn all you need to know about gut health and oral hygiene, including exactly how the two systems interact, symptoms of an optimally functioning gut and oral microbiome, plus five tips for protecting and prioritizing your gut and oral health.

Dr. Kami Hoss is a Dentist, Orthodontist, and Dentofacial Orthopedist with 24 years of dental experience. With his wife, Dr. Nazli Keri, they founded The Super Dentists. Their practice is one of the largest multi-specialty dental practices in Southern California. Dr. Hoss is the author of the #1 National Bestseller, “If Your Mouth Could Talk.”

What is a microbiome?
Because of its thrust into the buzzy, wellness zeitgeist, the term gut microbiome is thrown around often without little understanding of what it is—and the profound ways it impacts the body’s functioning. A microbiome is the collection of all microscopic organisms in a distinct environment. While the oral and gut microbiomes are separate systems, they work in tandem as a significant buffer through which the body filters through environmental inputs.
Why the Mouth-Gut Axis Should Be Top of Mind
“The oral microbiome, though less familiar to the general public compared to the gut microbiome, is a complex community of billions of microorganisms residing in the mouth,” notes Dr. Hoss. Of these, he cites bacteria, fungi, and viruses that inhabit different oral structures. Think: teeth, gums, and the tongue. Of course, the mouth is the first place that processes food. As such, “these microbes play a pivotal role” not only in how we digest food but also how our body protects against pathogens.
While many people consider symptoms of poor oral health like cavities and gum disease, a compromised oral microbiome can impact much more. Dr. Hoss explains that because the oral microbiome directly influences “overall digestive health and systemic wellness,” it’s imperative that we prioritize our oral hygiene.
The Relationship Between the Oral Microbiome and Gut
“A healthy oral microbiome can enhance gut microbial diversity,” says Dr. Hoss. But the inverse is also true—where an imbalance can “introduce pathogens to the gut, disrupting its function and potentially leading to gastrointestinal issues.”
Because these systems are so deeply interwoven and embedded in our body’s overall functioning, a weakened gut microbiome can also negatively impact the mouth. Dr. Hoss cites symptoms such as gum disease and cavities, “highlighting the bidirectional nature of the mouth-gut relationship.”
Signs of a Healthy Digestive System Within the Mouth
A healthy or compromised digestive system can manifest itself visibly in the mouth, helping to signify possible areas of concern.
Indicators of strong gut health in the oral cavity include:
Fresh breath Lack of chronic gum inflammation Robust teeth without excessive plaque Minimal occurrences of cavities“These signs suggest that the mouth is effectively managing its role as the entry point to the digestive system, where proper microbial balance is maintained and the initial breakdown of food occurs smoothly,” Dr. Hoss adds.
Conversely, signs that gut health is negatively impacting the oral cavity include:
Persistent bad breath (halitosis) Frequent dental cavities Gum inflammation Presence of oral lesions or ulcers“These issues can indicate imbalances or infections within the gut microbiome,” notes Dr. Hoss, “underscoring the systemic connection between gut health and oral conditions.”

7 Ways You Can Protect Your Gut Health and Oral Hygiene
As with many things whole-body health, maintaining good gut health and oral hygiene requires a holistic approach. Dr. Hoss encourages implementing the following habits to ensure these two systems function and operate their best. “By integrating these practices,” he notes, “including the use of carefully selected products like SuperMouth, one can ensure better oral and gut health, reflecting a more balanced microbial environment throughout the body.”
Consume a balanced, high-fiber diet to support a healthy microbiome. Practice rigorous oral hygiene and schedule regular dental check-ups. Stay hydrated to ensure adequate saliva production, which helps control oral bacteria. Choose oral care products wisely: for example, SuperMouth toothpastes and mouthwashes are formulated with ingredients like nano-hydroxyapatite and prebiotics, avoiding harsh antiseptics and essential oils that can decimate the oral microbes indiscriminately and disrupt the oral microbiome. Limit the use of antibiotics and products containing aggressive antimicrobials, including herbal ones such as peppermint oil, eucalyptus oil, and tea tree oil, which can harm beneficial bacteria. Manage stress, as it can influence both the microbiome and the immune system. Reduce sugary and acidic food intake to decrease the risk of bacterial overgrowth harmful to both oral and gut health.

 JimMin
JimMin 

























.jpg&h=630&w=1200&q=100&v=f776164e2b&c=1)






