Gaming the System: Cardiologists, Heart Stents, and Upcoding
Cardiologists can criminally game the system by telling patients they have much more serious, unstable diseases than they really have—fraud that results in unnecessary procedures, […]

Cardiologists can criminally game the system by telling patients they have much more serious, unstable diseases than they really have—fraud that results in unnecessary procedures, unnecessary costs, and unnecessary patient harm.
“The history of medicine abounds with dogmas assumed and later overcome”—sometimes, much later. The Women’s Health Initiative study showed that giving women Premarin, a hormone replacement therapy, increased the risk of the number one killer of women, heart disease, as well as breast cancer risk. Millions of women stopped taking it, and breast cancer rates came down.
Another such reversal of an established medical practice is percutaneous coronary intervention (PCI)—angioplasty and stents for stable coronary artery disease. Billions of dollars are spent on procedures shown “unequivocally” to offer no benefits.
So, why are cardiologists still doing them? Researchers did some focus groups and concluded: “Although cardiologists may believe they are benefiting their stable patients with CAD [coronary artery disease] by performing PCI, this belief appears to be based on emotional and psychological factors rather than on evidence of clinical benefits.”
“The sense of irrationality surrounding this practice is so strong that the phenomenon has been coined the oculostenotic reflex (I see a stenosis; I stent it).” They see a narrowing and stent it as though they can’t even help themselves.
Since the procedure carries some risks, including death, there’s an argument that stents should only be used for individuals who are actively having heart attacks and are in an emergency or unstable situation. Thankfully, there are now published, appropriate-use criteria in place to help guide cardiologists, and the good news is that 82 percent of stents are “reported to be performed in emergency or unstable situations.” So, we can disregard that ORBITA study that showed there was no benefit in stable patients since it’s now almost always performed only in unstable patients, right? Well, that’s how it’s almost always reported. “There are 2 ways a physician can become compliant. One is to do fewer unnecessary procedures”—which is the whole point (but where’s the money in that?)—“and the other is to make unnecessary procedures seem necessary.”
Is the implication that a doctor would try to game the system by telling a patient that they had a much more serious, unstable disease than they actually had, so the procedure could be carried out anyway? This is referred to as “upcoding.” Another word for it would be “fraud.” Researchers found that “some of that decline [in inappropriate use] may be driven by upcoding, falsely and intentionally misclassifying patients with stable angina as UA,” having unstable angina. As soon as those appropriate-use criteria went into effect, suspiciously, there was a four- to tenfold greater increase in rates of stents for acute coronary syndromes like heart attacks. “In New York, the proportion of PCIs labeled as acute, but performed as outpatient procedures, increased 14-fold…” There’s no biologically plausible reason why that would happen, so they were unnecessary procedures with unnecessary cost and unnecessary patient harm. And harm not only from the risk of getting an unnecessary stent but also from lying to the patient by exaggerating how bad their heart disease is. “This practice, at best, damages the credibility of the profession, increases health care spending, violates patient autonomy, puts the patient at risk of procedural complications and, at worse, may cross the threshold into criminal activity…”
What’s the solution? There could be an independent review panel to protect patients. “Simpler might be to remove the financial incentive to perform more procedures.”
“How many established standards of medical care are wrong? It is not known.” Bloodletting was the standard of care for thousands of years, for example. “Rigorous questioning of long-established practices is difficult. There are thousands of clinical trials, but most deal with trivialities or efforts to buttress the sales of specific products. Given this conundrum, it is possible that some entire medical subspecialties are based on little evidence.”
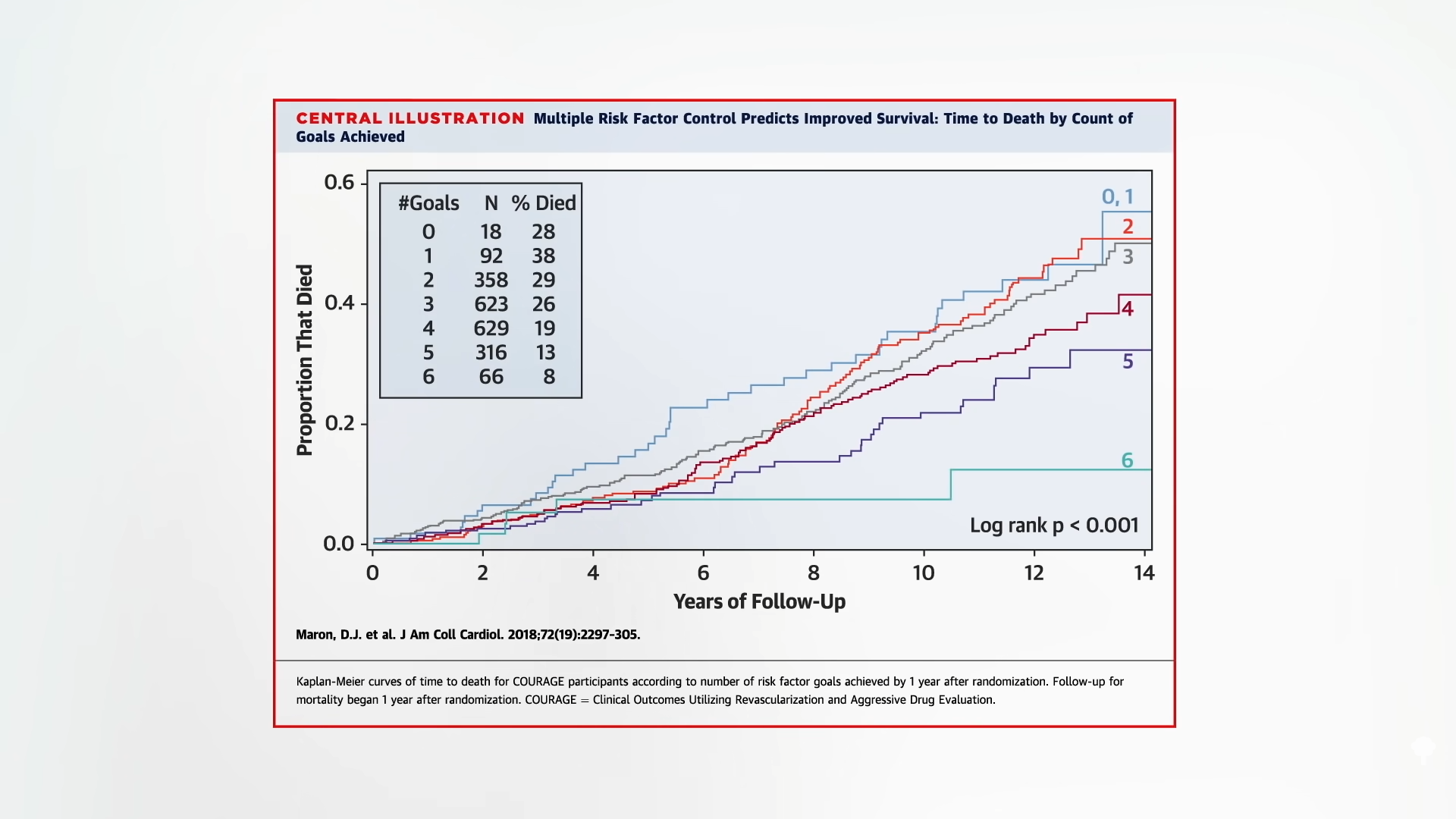
In the landmark COURAGE trial that showed stents were useless for extending life, what did seem to determine longevity? Ironically, in the case of heart stents, it was how many risk factors the patients were able to control. Those who achieved all six by lowering their blood pressure, cholesterol, weight, and smoking, while improving their diets and activity, had five times the survival over the subsequent 14 years than those who didn’t, as shown below and at 4:36 in my video Heart Stents and Upcoding: How Cardiologists Game the System.
Should we be surprised that angioplasty and stents fail to improve prognosis? After all, they do nothing to modify the underlying disease process itself. In other words, it doesn’t treat the cause. Even if stents helped with symptoms beyond the placebo effect, they would still just be treating the symptoms and not the disease. So, it’s no wonder the disease continues to progress until the patient is disabled to death. Dr. Esselstyn wrote, “Thus, the leading killer of men and women in Western civilization is being left untreated. What is being practiced is ‘palliative cardiology’: nontreatment of heart disease leading to disease extension and frequently an eventual fatal outcome.”
Deaths by the planeload every week, are “regarded as unfortunate,” rather than a national, preventable tragedy. “It is as though in ignoring this dairy, oil, and animal-based illness, we are wedded to providing futile attempts at temporary symptomatic relief”—rather than the cure.
Thankfully, “we are on the cusp of a seismic revolution in health…not another pill, procedure, or operation,” but instead treating the underlying cause of heart disease with whole food, plant-based nutrition, “the mightiest tool medicine has ever had in its toolbox.”
To get there, we need to fight a key nutrition deficiency in education. A study found that 90 percent of cardiologists reported receiving no or minimal nutrition education during their cardiology training, leaving fewer than one in ten feeling confident in their nutrition knowledge. So, maybe it’s a good thing that most spend just three minutes or less discussing nutrition with their patients. Only one in five cardiologists themselves even ate five servings of fruits and vegetables a day.
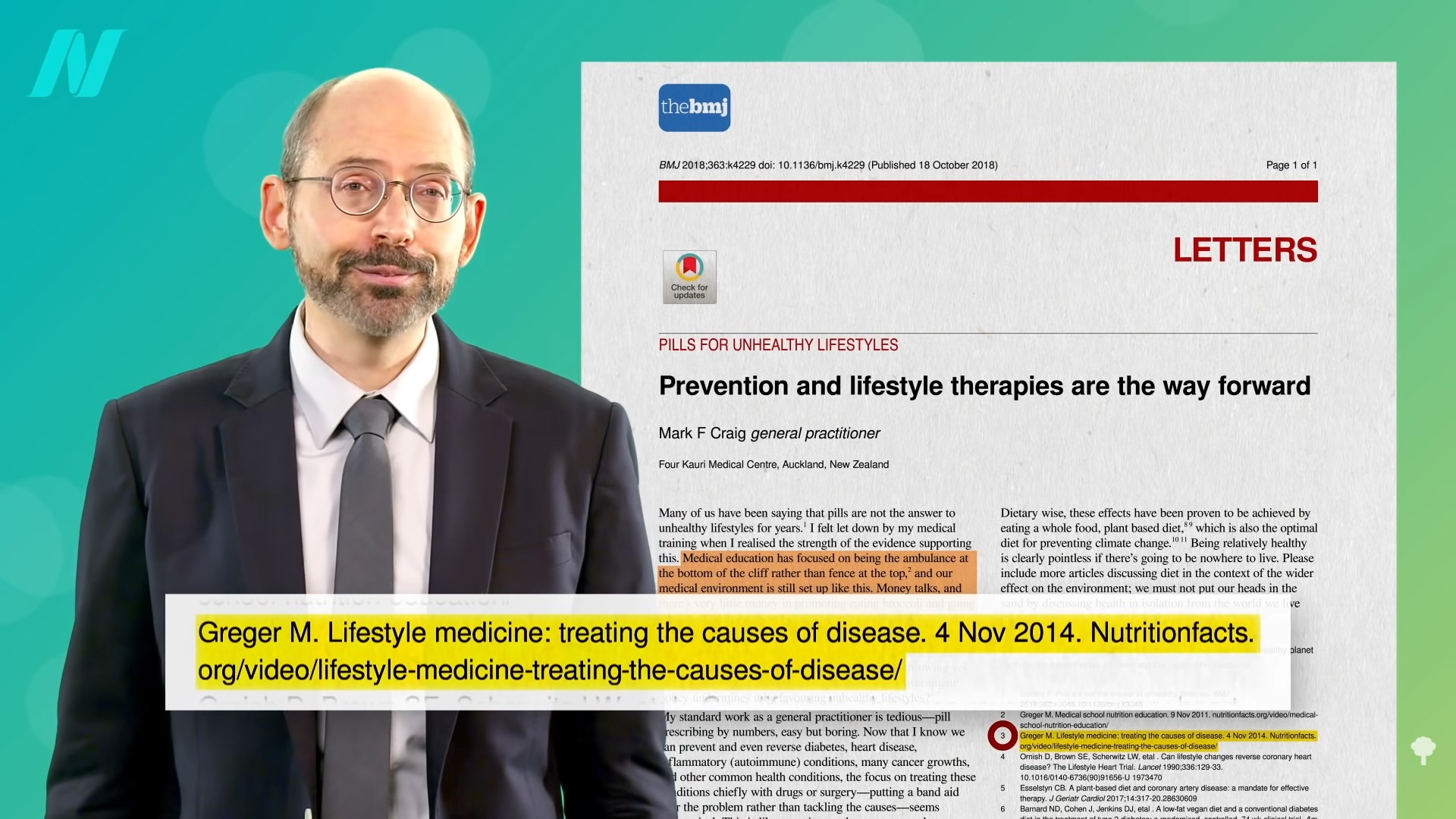
Thankfully, this lifesaving information is slowly but surely getting out there. “Medical education has focused on being the ambulance at the bottom of the cliff rather than a fence at the top. Money talks, and there’s very little money in promoting eating broccoli and going for a walk, despite them being much more effective.” I was so eager to see the citation they used for that and was so honored when I did, as shown below and at 7:14 in my video.

 Hollif
Hollif