How A Trip To The Eye Doctor Led Me To A Rare Autoimmune Disease Diagnosis
Living with chronic pain was never something I imagined for myself.

While some health issues are visible to the outside world, many people face chronic conditions that don't have externally visible signs or symptoms—also known as invisible illnesses. In mindbodygreen's new series, we're giving individuals with invisible illnesses a platform to share their personal experiences. Our hope is their stories will shed light on these conditions and offer solidarity to others facing similar situations.
Living with chronic pain was never something I imagined for myself, especially when I was in my early twenties. I was young, taking care of myself, and didn't have a care in the world when it came to my health. Sure, my joints were pretty poppy, and my hands would get inflamed seemingly out of nowhere, but that was normal right? Not exactly.
My symptoms became impossible to ignore
Back in the beginning of the pandemic, I started noticing more and more little things that felt off in my body. Maybe it was the fear the pandemic instilled, but I became convinced something was wrong, even though friends and family tried to assure me I was fine.
My eyes were constantly sore and bloodshot, my muscles felt weak, and my back ached on and off. I attributed most of it to sitting a lot while working and not getting as much movement because of quarantine. I did, however, want to investigate the problem with my eyes.
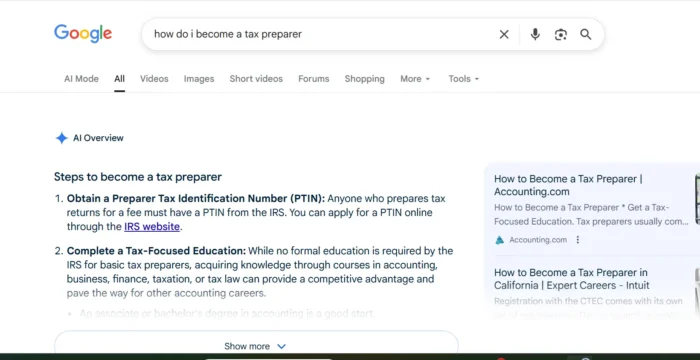
When none of the eye drops I was prescribed helped, my optometrist mentioned the word "lupus," and said I should see my primary care provider—so off I went. When bloodwork came back showing an elevated inflammatory marker, the next course of action was to see a rheumatologist.
After x-rays, ultrasounds, and one excruciatingly long MRI, my rheumatologist finally had answers for me.
Finally getting a diagnosis
There's nothing quite like waiting on important medical results, and if you've never experienced it, I hope you never have to. I'll always remember how it felt logging on to that e-visit with my rheumatologist, knowing it could be a life-changing conversation—and it was.
The MRI showed I had a point of inflammation in my right hip. That, along with the other symptoms I was experiencing, brought my rheumatologist to a conclusion.
"It's something called ankylosing spondylitis," he said over the video call. The rest of the conversation was a blur, to be honest. He told me information about the disease: It's an autoimmune condition similar to rheumatoid arthritis, but it's concentrated in the spine. And, if it progresses, it can eventually lead to fusion of the spinal vertebrae. It's rare, he said, and it's significantly more common in men. (Cool.)
After over two months of tests and appointments, I was ultimately relieved to have an answer—and to know I wasn't imagining things. And though it is a lifelong condition with no known cure, I was also relieved it wasn't anything terminal—but that certainly didn't mean I was happy.
The months following my diagnosis were difficult and dark. There was a part of me that denied it, a part of me that was mad at myself for succumbing to an autoimmune condition, and a part of me that felt weirdly inspired by the opportunity to learn how to manage it.
After all, I was (and still am) a certified yoga instructor working for a health and well-being company—how could I have let this happen? And more importantly, how could I heal myself?
The truth is, I didn't "let" anything happen, and the reality that I might never eradicate my symptoms was difficult to accept. Stories of remission were slim, and with ankylosing spondylitis being so rare, resources and research were relatively limited.
There was always, of course, biologics, my rheumatologist assured me. They're a type of drug that stop inflammation from wreaking havoc on your body—at the cost of shutting your immune system down. And if there was ever a time I didn't want to go on immunosuppressants, it was the beginning of the pandemic, for obvious reasons.
So, I started to learn more about ankylosing spondylitis, autoimmune conditions in general, and how other people were managing. Scouring Facebook pages, blogs, and research, I discovered what was working for some people: plenty of movement, managing stress, and an anti-inflammatory diet (namely, avoiding starchy or glutenous foods), among other things.
Let me start by saying I have, by no means, figured out a foolproof system for managing my AS. I still have flares, and my back does still bother me. But almost two years since receiving my diagnosis, I definitely have a better handle on it now than I once did.
Diet and exercise, specifically, have proven to be important factors in fending off flares. When I do eat certain things—like sugar, refined oils, alcohol, and gluten—sure enough, my symptoms flare. I'm also noticeably more stiff when I don't get enough exercise, or sit for long periods of time. So, I do my best to stay on top of my movement routine.
But the biggest inflammatory trigger of them all, at least for me, has been stress. When my fight or flight kicks in, I get those telltale, hot, red, puffy hands, and the effects ripple out through my body. I developed a newfound curiosity for the mind-body connection, which led me to a therapist who specializes in chronic pain. Working with her has been extremely helpful in not only learning how to manage stress, but working on some of the underlying issues that spike my stress levels.
Ultimately, my main focus now is maintaining homeostasis in my mind, body, and spirit. Lifestyle is key—but to that end, trying not to worry about getting it perfect 100% of the time is important, too. Sometimes I think the stress of trying to heal does more harm than good.
So, I do my best to hold myself accountable with grace, and also stay realistic. Will I ever experience remission? I don't know. And if it gets to the point where biologics are the only option to keep my spine healthy, I'll cross that bridge when I come to it. I do hope more treatment options become available, though, as we start to understand autoimmunity more.
What I want people to know
Having an invisible and/or chronic illness of any kind can feel isolating, defeating, and deeply upsetting, so if there's anything I want people to know, it's that you are not alone in your struggle. In fact, the unfortunate reality is, more and more people are being diagnosed with autoimmune conditions.
There is no shame in receiving a diagnosis, and there is no shame in talking about what you're going through with your support system. And if those in your life can't relate, find people who do, so you can lean on each other in times of need.
Autoimmunity is still deeply misunderstood, and until we have more answers as to what causes it and how to cure it, the best we can do is take care of ourselves, stay up to date on the research, and listen to our bodies. In the words of late educator and author, Randy Pausch, "We cannot change the cards we are dealt, just how we play the hand."

 Kass
Kass